Adolescents have a delayed sleep clock
There are two reasons adjusting school start times for middle and high school students is important for the health, safety and success of our Minnesota teenagers : 1) to allow them to obtain the recommended amount of sleep (8-10 hours) and 2) to accomplish this by timing the opportunity for sleep in sync with the natural developmental shift in their sleep schedule.
Extensive research in the timing of the brains sleep clock suggests a strong role for a natural delay in bed time and awakening time. Although other effects such as inheritance [such as tendency to be a night owl or an early bird], and habits [such as light exposure from electronic device use and caffeine use] are important, neither comes into such direct conflict with natural sleep rhythm as typical American school schedules. Across cultures, after the age of 12, all children experience natural changes in clock timing and their adolescent sleep schedule becomes delayed. Although sleep behaviors and inheritance might play a role in an individual adolescent’s experience, early school start times reduce the amount of sleep by forcing adolescents into schedules that are in conflict with natural sleep schedules.
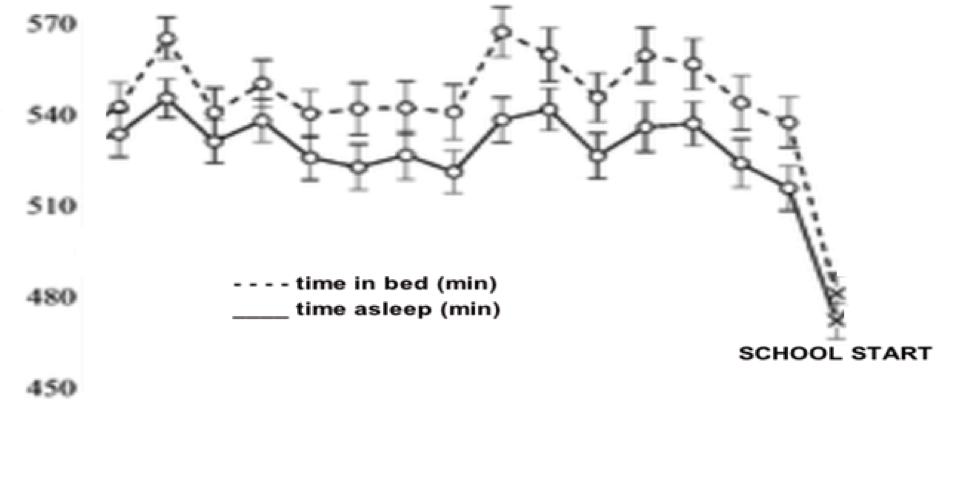
As shown in the graph, this “crash” into school schedules results in an immediate sleep loss reported to result in a one hour nightly drop from nearly 9 hours (540 minutes) sleep in the summer to less than 8 hours (480 minutes) on weekdays when school starts.
Teenagers sleep best between the hours of 10:45 p.m. to 8:00 a.m. |
It might help to think of teenagers as sleeping in a completely different time-zone than everyone else. |  |
Teens are not getting enough sleep
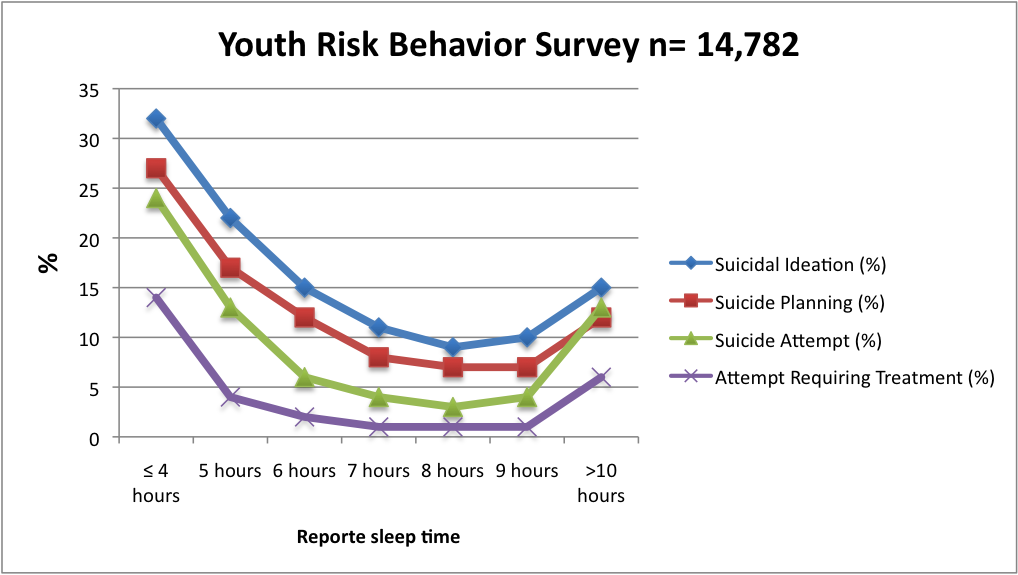
The most immediate impact of early school start time is chronic insufficient sleep during the academic school year. Every two years, the CDC has been gathering data on U.S. teenage sleep duration. Data from 50,370 high school students collected from 2007-2013 revealed insufficient sleep ranged from 60% of students in 9th grade to 77% of students in 12th grade. Those students who reported insufficient sleep (< 7 hours) were more likely to report risk taking behaviors, a finding consistent with numerous other studies. The biologic consequences of insufficient sleep include emotional dysregulation, impaired judgement, and risk taking. Adolescents with insufficient sleep are more likely to have car accidents, to use alcohol and drugs, and based on a survey in the Fairfax Virginia school district, nearly 7 times more likely to attempt suicide from 1.% of those meeting recommended 9 hours of sleep to 14% of those getting 4 hours or less of sleep:
Benefit of later school start times
Standards of evidence for validating medical decisions relies on randomized trials of drugs or other therapies, often in small, highly selected populations in very controlled circumstances that may not always be generalizable to real-world circumstances. By example, the current medical evidence for changing light exposure habits narrowly targeted to improve sleep time encompasses only 171 patients studied during brief experimental conditions.
By contrast, public policy recommendations such as optimal school start time cannot be easily estimated using standard randomized controlled trials and is better positioned in the real-world context with observations of populations that capture the impact over prolonged periods of time. Nineteen studies, including longitudinal studies of more than 70,000 students, show that sleep duration increases with later school start times and also show greater effects the later the start time. This increased sleep duration with later school start times shows increasing benefits in emotional regulation and depression, safety and risk-taking, cognitive and academic performance, and even athletic performance. Current evidence from these studies supports reduction in car accidents, improved mood, improved attendance and alertness in class and less tardiness. Follow the links to learn more about these benefits.
- Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, Lloyd RM, Malow BA, Maski K, Nichols C, Quan SF, Rosen CL, Troester MM, Wise MS. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med 2016;12(6):785–786.
- Wheaton, A. G., Chapman, D. P. and Croft, J. B. (2016), School Start Times, Sleep, Behavioral, Health, and Academic Outcomes: A Review of the Literature. J School Health, 86: 363–381. doi:10.1111/josh.12388
- Hagenauer MH, Perryman JI, Lee TM, Carskadon MA. Adolescent Changes in the Homeostatic and Circadian Regulation of Sleep. Developmental Neuroscience. 2009;31(4):276-284. doi:10.1159/000216538.
- Russo, P. M., Bruni, O., Lucidi, F., Ferri, R. and Violani, C. (2007), Sleep habits and circadian preference in Italian children and adolescents. Journal of Sleep Research, 16: 163–169. doi:10.1111/j.1365-2869.2007.00584.x
- Carskadon MA1, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. .Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998 Dec 15;21(8):871-81
- Bei, B., Allen, N. B., Nicholas, C. L., Dudgeon, P., Murray, G. and Trinder, J. (2014), Actigraphy-assessed sleep during school and vacation periods: a naturalistic study of restricted and extended sleep opportunities in adolescents. J Sleep Res, 23: 107–117. doi:10.1111/jsr.12080
- Wheaton AG, Olsen EO, Miller GF, Croft JB. Sleep Duration and Injury-Related Risk Behaviors Among High School Students — United States, 2007–2013. MMWR Morb Mortal Wkly Rep 2016;65:337–341. doi: http://dx.doi.org/10.15585/mmwr.mm6513a1
- McMakin, D. L., Dahl, R. E., Buysse, D. J., Cousins, J. C., Forbes, E. E., Silk, J. S., Siegle, G. J. and Franzen, P. L. (2016), The impact of experimental sleep restriction on affective functioning in social and nonsocial contexts among adolescents. J Child Psychol Psychiatr, 57: 1027–1037. doi:10.1111/jcpp.12568
- Mike, Thomas B. et al. The hazards of bad sleep—Sleep duration and quality as predictors of adolescent alcohol and cannabis use. Drug & Alcohol Dependence , Volume 168 , 335 – 33
- Winsler, A., Deutsch, A., Vorona, R.D. et al. J Youth Adolescence (2015) 44: 362. doi:10.1007/s10964-014-0170-3
- L Rychetnik, M Frommer, P Hawe, A Shiell. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health 2002;56:119-127 doi:10.1136/jech.56.2.119
